In a world where health awareness is paramount, understanding the early warning signs and symptoms of diabetes can be a lifesaving skill. This article serves as a comprehensive guide, shedding light on the subtle yet crucial indicators of diabetes and offering insights into the significance of early detection. Whether you are seeking information for yourself or a loved one, this resource will empower you with the knowledge needed to recognize the red flags of diabetes and take proactive steps toward a healthier future.
Table of Contents
Understanding Types of Diabetes
Diabetes is a group of disorders that affect the body’s ability to regulate blood sugar (glucose) properly. This regulation is largely controlled by the hormone insulin, which is produced by the pancreas. There are several forms of diabetes, with Type 1 and Type 2 being the most common.
Type 1 Diabetes
Type 1 diabetes, often diagnosed in childhood or adolescence, is an autoimmune diabetes where the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Individuals with Type 1 diabetes are dependent on insulin injections or an insulin pump to manage their blood sugar levels. This type is relatively rare, accounting for about 5-10% of all diabetes cases. Environmental factors also play a crucial role in this type of diabetes.
Type 2 Diabetes
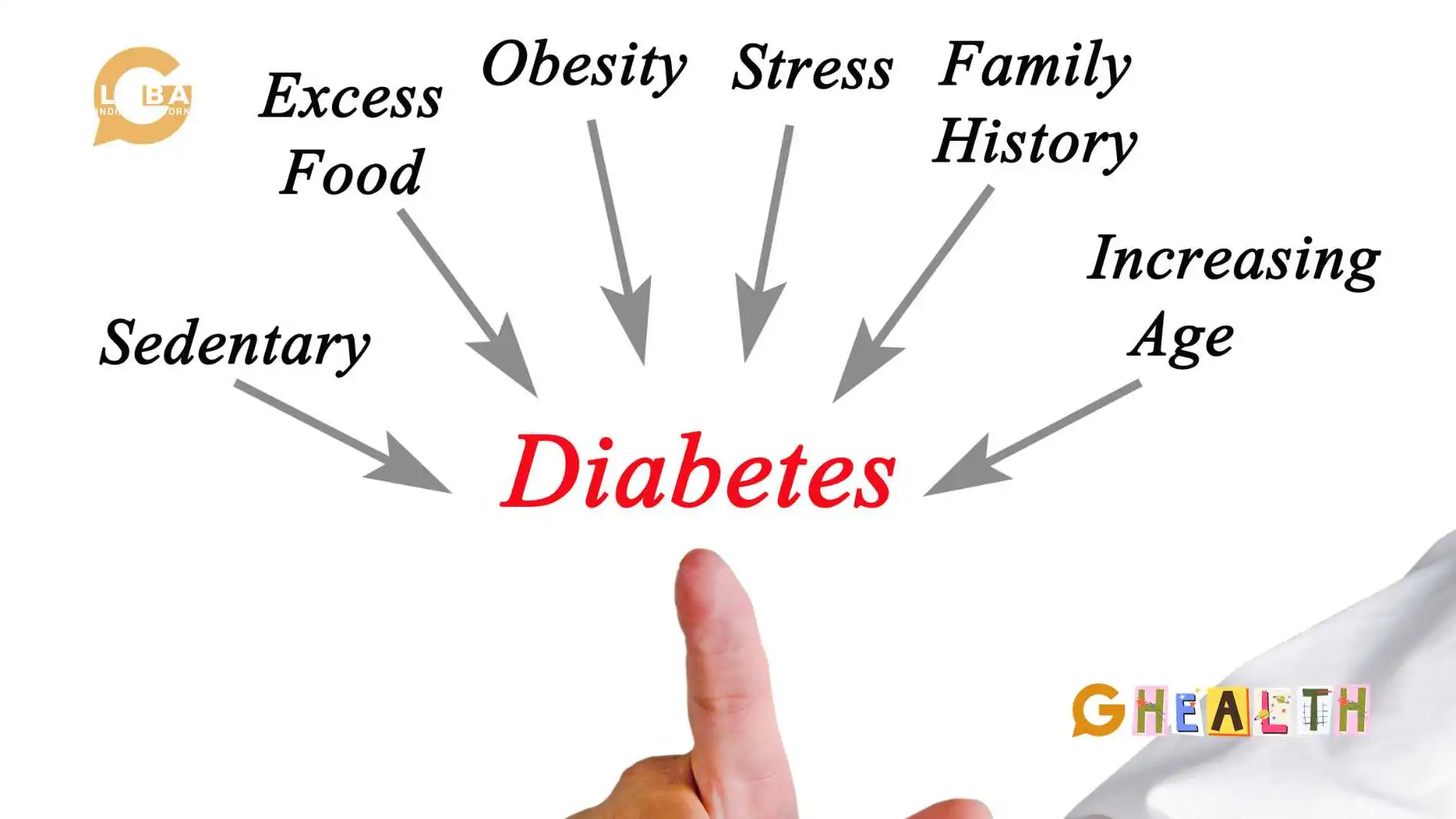
People with Type 2 diabetes is a more common type and typically develops in adulthood, although it can occur at any age. It is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, and the pancreas eventually fails to produce enough insulin. Lifestyle factors, such as poor diet, lack of physical activity, and obesity, play a significant role in the development of Type 2 diabetes. It accounts for the vast majority of diabetes cases, approximately 90-95%. It is also called Diabetes Mellitus.
Gestational Diabetes
Gestational diabetes is another type of diabetes that occurs during pregnancy. It affects some women who did not have diabetes before becoming pregnant. The condition results from hormonal changes that affect insulin’s effectiveness, leading to elevated blood sugar levels. Managing gestational diabetes is crucial to ensure the health of both the mother and the baby. This typically involves dietary changes, regular monitoring of blood sugar levels, and, in some cases, medication.
Most women with gestational diabetes return to normal blood sugar levels after giving birth, but it increases the risk of developing Type 2 diabetes later in life. Therefore, affected individuals need to maintain a healthy lifestyle and undergo postpartum screening for diabetes.
Early Warning Signs and Symptoms
The signs and symptoms of diabetes can be subtle and often go unnoticed, especially in the early stages. However, it’s crucial to be aware of these indicators to help early detection, lower the risk of Type 1 and Type 2 diabetes, and timely intervention. The symptoms and signs of Type 1 and Type 2 diabetes include:
Hunger and Weight Changes
One of the earliest signs of diabetes, both Type 1 and Type 2, is increased hunger (polyphagia) and unexplained weight changes. Here’s how these symptoms manifest:
Increased Hunger: People with diabetes may experience excessive hunger, even shortly after eating a meal. This results from the body’s inability to effectively use glucose for energy, leading to a constant feeling of hunger.
Weight Loss (in Type 1) or Weight Gain (in Type 2): In people with Type 1 diabetes, unexplained body weight loss is often a noticeable symptom. The body breaks down muscle and fat for energy when it cannot use glucose, resulting in rapid weight loss. In contrast, Type 2 diabetes may lead to weight gain, as insulin resistance can cause higher blood glucose levels; this excess glucose is stored as fat. This weight gain is particularly evident in the abdominal area.
It’s important to note that while increased hunger is a common early sign, it can also be attributed to other factors such as stress, a high metabolic rate, or dietary habits. Weight changes may also result from various factors. Hence, these symptoms should be considered alongside other signs of diabetes for a comprehensive evaluation.
Frequent Urination and Excessive Thirst
The second set of early warning signs relates to changes in urination and thirst patterns, which are closely interlinked.
Frequent Urination (Polyuria): High blood sugar levels lead to increased glucose levels in the urine, which draws more water from the body. This results in frequent urination. People with diabetes may find themselves needing to urinate more often, both during the day and at night.
Excessive Thirst (Polydipsia): Frequent urination causes a loss of fluids, leading to dehydration. Dehydration triggers extreme thirst as the body attempts to compensate for losing fluids. The connection between frequent urination and excessive thirst is a hallmark of diabetes. It’s essential to be vigilant about changes in these patterns, mainly when they occur together, as they are often strong indicators of elevated blood sugar levels.
Additional Symptoms
In addition to hunger and weight changes, frequent urination and excessive thirst, there are several other common symptoms of type 1 and 2 that may signal the presence of diabetes. These classic symptoms include
- Fatigue: People with diabetes may experience unexplained fatigue due to the body’s inability to utilize glucose for energy properly. They also manifest itchy skin. A condition called Acanthosis Nigrican where the skin around the armpits and neck change colour.
- Blurred Vision: High blood sugar levels can cause changes in the shape of the eye’s lens, leading to blurry vision or vision loss.
- Slow Healing: Diabetes can impair the body’s ability to repair and regenerate tissues, resulting in slower wound healing and frequent skin infections.
- Numbness and Tingling: Elevated blood sugar levels can damage blood vessels and nerves, leading to peripheral neuropathy, which causes numbness and tingling, particularly in the extremities.
- Recurrent Infections: High blood sugar can weaken the immune system, making individuals with diabetes more susceptible to infections, such as urinary tract infections, skin infections, yeast, and fungal infections.
It’s important to note that some symptoms may vary between Type 1 and Type 2 diabetes. For instance, unexplained weight loss is a more common sign of Type 1 diabetes, while weight gain is often associated with Type 2 diabetes. However, many symptoms are shared between the two types, making it crucial to consult a healthcare professional for a proper diagnosis.
Complications of Diabetes
Diabetes is a chronic disease that can lead to a range of complications, especially when blood sugar levels are not well-controlled over an extended period. These diabetes complications can affect various organs and systems in the body and can be severe complications. The primary risk of complications of diabetes in adults and risk factors for Type 1 and Type 2 diabetes include:
Cardiovascular Disease
Cardiovascular disease encompasses conditions such as heart disease, heart attack or stroke, and peripheral artery disease. People with diabetes are at a significantly higher risk of developing these conditions due to factors like elevated levels of glucose, high blood pressure, and abnormal cholesterol levels. It’s the leading cause of death among individuals with diabetes.
Diabetic Retinopathy
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the eye’s retina. It can lead to vision problems and even blindness if left untreated. Regular eye exams and blood sugar control are crucial in preventing and managing this condition.
Diabetic Nephropathy
Diabetic nephropathy is kidney damage caused by prolonged high blood sugar levels. It is a leading cause of kidney failure. Early detection through regular urine and blood tests, along with strict blood sugar control, can help delay or prevent the progression of kidney diseases.
Diabetic Neuropathy
Diabetic neuropathy is nerve damage resulting in numbness, tingling, pain, and muscle weakness, typically in the extremities. This condition can also affect the digestive system, heart, spinal cord, and other organs. Good blood sugar control and medications to manage neuropathic pain can help alleviate symptoms.
Diabetic Foot Ulcers
Diabetic foot ulcers are open sores that commonly develop on the feet due to nerve damage and poor blood circulation. Left untreated, they can become infected and may lead to severe complications, including the need for amputation. Proper foot care, regular check-ups, and managing blood sugar levels are essential in preventing and managing diabetic foot ulcers.
Diagnosis and Testing
Recognizing the early warning signs is the first step toward managing diabetes. However, a formal diagnosis of diabetes should be made by a healthcare provider through the following methods:
- Fasting Blood Sugar Test: This test measures blood sugar levels after an overnight fast. A fasting blood sugar level of 126 milligrams per deciliter (mg/dL) or higher indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): After an overnight fast, a glucose solution is ingested, and blood sugar levels are tested at intervals. A two-hour blood sugar level of 200 mg/dL or higher suggests diabetes.
- Hemoglobin A1c Test: This test measures the average blood sugar level over the past two to three months. An A1c level of 6.5% or higher is diagnostic of diabetes.
- Random Blood Sugar Test: A random blood sample is taken at any time, and a blood sugar level of 200 mg/dL or higher, along with classic diabetes symptoms, indicates diabetes.
- Antibody Tests (for Type 1): In cases where Type 1 diabetes is suspected, antibody tests can confirm autoimmune destruction of beta cells in the pancreas.
Treatment and Management
Once diagnosed, individuals with diabetes must take steps to manage their health condition effectively. The treatment for Type 1 and Type 2 diabetes are:
- Type 1 Diabetes:
- Management involves daily insulin injections or using an insulin pump to replace the insulin the body no longer produces.
- Monitoring blood sugar levels regularly is crucial to adjust insulin doses accordingly.
- Lifestyle modifications, such as a healthy diet and regular exercise, are essential for healthy life.
- Type 2 Diabetes:
- A sedentary lifestyle triggers Type 2 diabetes. This includes adopting a balanced diet, regular exercise, and weight management.
- Some individuals may require oral medications or insulin injections to help regulate blood sugar levels.
- Treatment of Type 2 diabetes is regular monitoring of blood sugar levels and annual check-ups for long-term management.
Conclusion
Early intervention is key to effectively managing and mitigating the impact of diabetes, ensuring a healthier and more fulfilling life for individuals at risk. Individuals can seek timely medical attention, enabling better control of their health and a reduced risk of diabetes-related complications. Early warning signs and symptoms of diabetes serve as vital cues for timely intervention and improved overall well-being.
FAQs
What drink lowers blood sugar?
Water and herbal teas, such as cinnamon tea or green tea, can help lower blood sugar levels by promoting hydration and potentially improving insulin sensitivity.
What foods are bad for diabetics?
Foods high in added sugars and refined carbohydrates, like sugary drinks and white bread, can be harmful for diabetics as they can cause rapid blood sugar spikes. High-fat, processed foods should also be limited as they can lead to weight gain and worsen insulin resistance.
What foods are good for diabetics?
For diabetics, fibre-rich foods, like vegetables, whole grains, and legumes, are excellent choices as they help stabilize blood sugar levels. Additionally, lean proteins and healthy fats, such as those found in fish, nuts, and avocados, can support balanced blood sugar and overall health.
How to avoid diabetes?
To reduce the risk of developing diabetes, maintain a healthy weight through a balanced diet and regular physical activity.